We use cookies to enhance your browsing experience and analyze the performance of our website. By clicking Continue, you agree to the use of cookies. For more information, please see our Privacy Policy or update your Cookie Preferences.


In recent years, researchers have uncovered a fascinating connection between gut health and hormones. The gut, often called the "second brain," plays a crucial role in regulating the balance of hormones like estrogen, thyroid, cortisol, and insulin. This blog explores the intricate relationship between gut health and hormones, shedding light on how imbalances in the gut can lead to hormonal issues. You'll also learn practical tips for maintaining a healthy gut to support overall well-being.
The gut and hormones are interconnected through a complex network known as the gut-brain axis. This communication highway allows the gut and brain to send signals to each other, influencing various bodily processes, including hormone regulation.
One of the key players in this communication network is the gut microbiome, a vast community of trillions of bacteria that reside in the digestive tract. These bacteria play a crucial role in breaking down food, producing essential nutrients, and modulating the immune system. Emerging research suggests that the gut microbiome also plays a role in regulating hormones.1
While the gut microbiome impacts hormone levels, hormones themselves also regulate gut function. This is shown by differences in the gut microbiomes of males versus females, where estrogen and testosterone play an important role in regulating the composition of the gut microbiome.2 Furthermore, progesterone is protective in the gut by decreasing intestinal permeability (leaky gut) and gut inflammation.3
There are many ways that poor gut health can lead to hormone imbalances.
When the gut microbiome is out of balance, known as dysbiosis, it can have far-reaching effects on hormone levels. Dysbiosis can lead to increased gut permeability, also known as leaky gut, allowing toxins, bacteria, and undigested food particles to enter the bloodstream. This can overwhelm the immune system and cause the immune system to start attacking your own body, also known as an autoimmune response. A leaky gut can pave the way to these autoimmune reactions, leading to inflammation, which in turn can disrupt hormone production and balance.2
For example, autoimmune thyroid diseases can lead to imbalances of thyroid hormones. Again, these autoimmune thyroid diseases, such as Hashimoto's thyroiditis and Graves' disease, may have originated with a leaky gut.4 Healing the gut can help tamper the autoimmune response and improve symptoms.5
Another hormone particularly affected by poor gut health is cortisol, the body's primary stress hormone. Chronic stress and cortisol can disrupt the gut microbiome through multiple pathways, leading to dysbiosis and leaky gut. A vicious cycle ensues, and microbes in the gut can activate stress circuits in the nervous system and brain.6 This can contribute to a host of health issues, including weight gain, fatigue, and mood disorders.
Additionally, imbalances in gut bacteria can impact the key hormone insulin, involved in blood sugar balance. Insulin resistance, often associated with obesity and type 2 diabetes, can be exacerbated by poor gut health, highlighting the importance of a healthy gut microbiome in maintaining overall metabolic health. Less diverse microbiomes are associated with insulin resistance.7 Researchers suggest that short-chain fatty acids, bacterial byproducts produced from fiber, may be involved in improving insulin resistance.8
Many hormones and harmful toxins are detoxified by the liver, and then dumped into the GI tract for elimination with each bowel movement. As the hormones and toxins pass through the intestines, they encounter the gut bacteria. Gut bacteria produce an enzyme called beta-glucuronidase. If too much of this enzyme is present, it can actually result in the reuptake of hormones and toxins back into the body!
A lot of research centers around estrogen processing by the gut microbiome, referred to as the 'estrobolome' - you can see a visual of how the estrobolome works in the graphic below. If too much estrogen is absorbed back into the body, it may result in estrogen-dominant conditions such as endometriosis, polycystic ovarian syndrome (PCOS), and breast cancer.19 If you've ever had high estrogen on testing, it might be helpful to test stool beta-glucuronidase to see if this is the reason why.
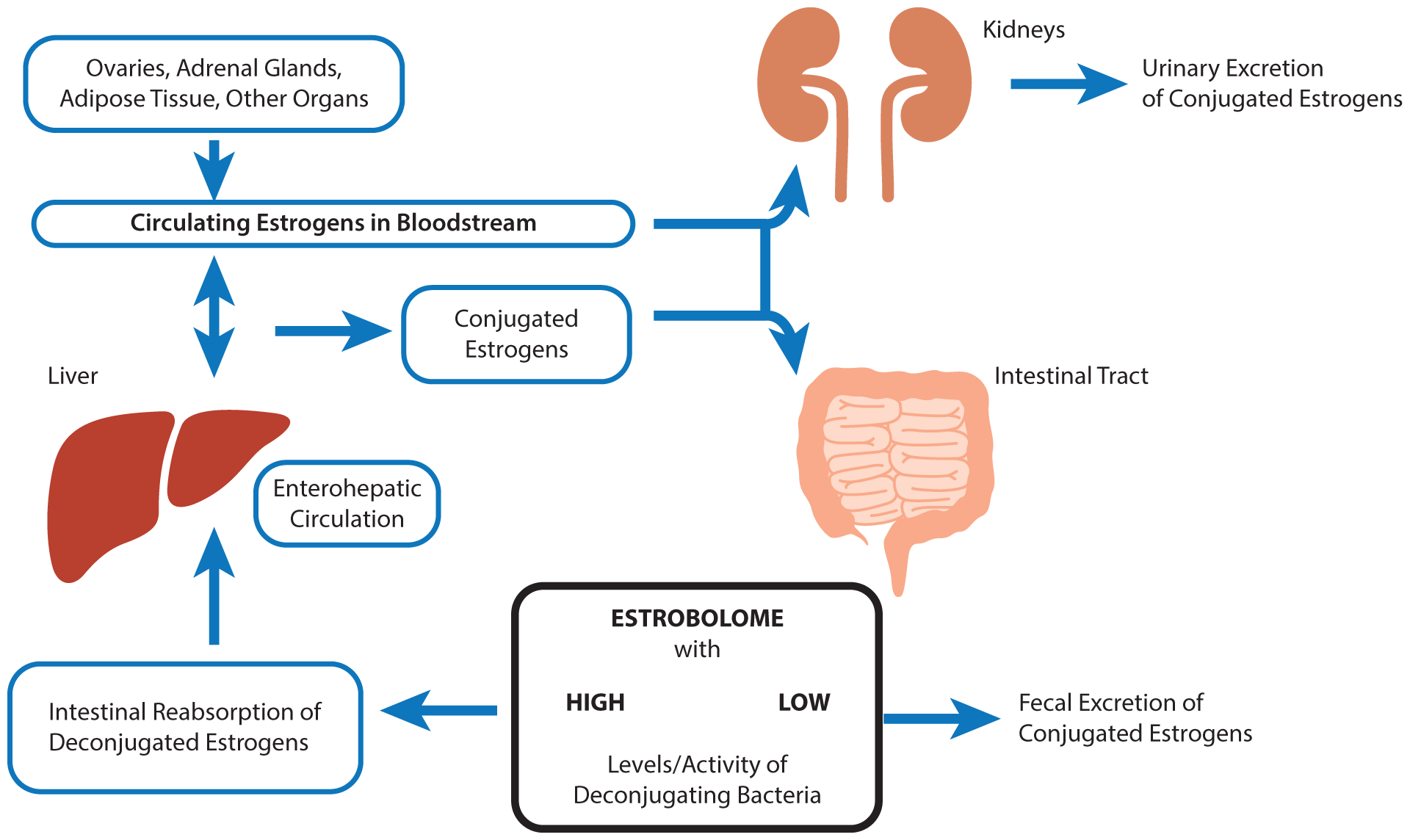
In addition to estrogen, other hormones that are detoxified through liver glucuronidation pathways are thyroid, melatonin, testosterone, and vitamin D (yes, vitamin D is both a vitamin AND a hormone)!10 These hormones also have the potential for reactivation when the microbiome is imbalanced and beta-glucuronidase levels are elevated.
Fortunately, there are 4 simple steps you can take to improve your gut health and support hormonal balance.
In conclusion, the gut plays a crucial role in regulating hormones and maintaining gut health is essential for overall well-being. By adopting a gut-friendly diet and lifestyle, you can support a healthy gut microbiome and promote hormonal balance.
If you'd like to learn more about beta-glucuronidase and hormones, and how to address abnormal levels, check out "What is Beta-Glucuronidase and Why Should You Care?" from The Lab Report. Our podcast is a great way to learn more about functional medicine and address the root causes of disease.
This article is meant for educational purposes only and is not meant to be misconstrued as medical diagnosis or treatment advice.